mCoder: AI-Powered Autonomous Medical Coding
85% Direct-to-Bill Rate
Code reports in seconds—no human intervention, no backlog. mCoder reads clinical documentation, assigns accurate CPT®, HCPCS, and ICD-10-CM codes, and sends 85%+ claims straight to billing. Expect 24/7 throughput, faster cash flow, and fewer denials from day one. Transform revenue cycle management with AI-powered precision.
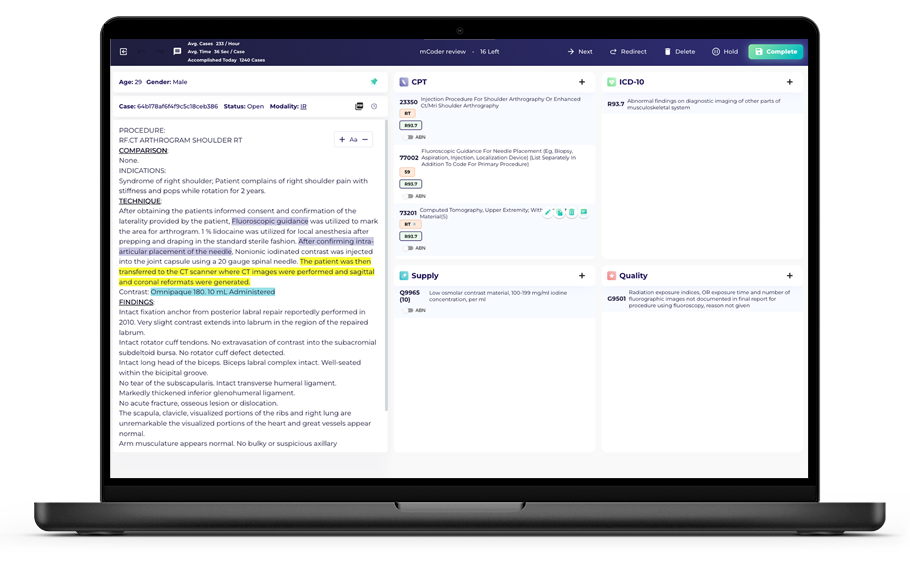
How it Works
mCoder’s engine is trained on two years of your documentation and coding history – learning patterns, payer mix, and policies to deliver high direct-to-bill performance from day one. The technology combines machine learning, deep learning, and transformer models to understand full-report context-not just keywords-and assigns codes automatically, without human intervention. The engine sends the vast majority of bases straight to billing. Incomplete, complex, or low-confidence reports are intelligently routed to your team for manual review and coding in the mCoder platform. Every action is transparent and trackable in the mCoder dashboard—giving you full visibility into throughput, accuracy, and exception handling.

Key Outcomes at Go-Live
85%+ Direct-to-Bill on Day 1
Returns codes in as little as two seconds
Operate with zero backlog; accelerate billing cycles and cash flow
Why Customers Love It

Tailored to your workflow
Learns your coding standards, report templates, payer rules, and site makeup for consistent, compliant outcomes.

Always up-to-date
Stays current with evolving CPT®, HCPCS, and ICD-10 code sets and policy updates.
Clarity and control
Built-in explainability shows exactly which documentation supported each code, and all DTB encounters remain fully reviewable.

Live monitoring and accessible KPIs
The mCoder dashboard is at your fingertips 24/7. Track DTB rate, accuracy rate, and other metrics any time you want.
Imaging center network achieves 87% DTB rate in under 90 days
Customer: The Nationwide Imaging Network
- Over 100 sites
- Over 1.5 million scans each year
- Multiple states
The Challenges
- Limited coding staff
- Rapid growth trajectory
- Coding bottlenecks and backlogs
- Growing denials
Results with mCoder
- 87% DTB rate
- 95% coding accuracy
- 60% budget savings
- Unlimited scale without any additional staffing
SDMI Accelerates Billing & Eliminates Coding Delays
The Customer: Steinberg Diagnostic Medical Imaging
- 500,000+ studies annually
- Multiple sites
- Leading outpatient provider
The Challenges
- 10-12 day coding lag time
- Slowed billing & revenue capture
- 40% baseline automation for high-volume studies
Results with mCoder
- Achieved 85% DTB rate
- Reduced lag time to 1 Day
- Eliminated need for outsourcing
Implementation & Support
![]()
Rapid implementation: Customers go live within ~90 days. Our structured process achieves 85% DTB on Day 1. Maverick works with you to closely monitor coding accuracy and conducts quarterly audits to ensure sustained accuracy.
![]()
Support you can count on: Dedicated account manager, real-time dashboards, and responsive help desk with prioritized handling of critical issues.
Security is Our Priority
HIPAA compliant and SOC 2 certified, with encryption in transit and at rest, role-based access, audit logging, and continuous monitoring on U.S.-based AWS infrastructure.
How mCoder Works
Ready to Leverage AI for your Coding?
Use our Vendor Evaluation Tool—with standardized criteria and side-by-side comparison—to confidently assess autonomous coding solutions.
- Accelerate understanding of essential criteria
- Make confident, data driven decisions
- Align stakeholders faster with a shared tool
- Ensure solution fit with your organization’s priorities

This project was important to help support our team with areas that are out of their control and bring attention to conversations across the organization to find solutions. It is important to remember this is an ongoing project that reaches across many, including Radiologists, PACS Administrators and business analysts to help move the needle toward increased DTB.
— Rachel Papka, Chief Innovation Officer, SDMI
![]()
How is autonomous medical coding different from computer-assisted coding (CAC)?
![]()
CAC suggests codes for humans to finalize; autonomous coding completes the process end-to-end, enabling high DTB rates that traditional CAC struggles to achieve. Read more about the advantages of autonomous coding.

